How airborne particle counters provide vital information for IAQ in healthcare facilities
In the highly sensitive environment of a healthcare facility, where both infection patients and those highly susceptible to infection receive treatment, it is essential to minimize the possibility of infection and disease transmission.

Using a Fluke particle counter to test indoor air quality in a healthcare facility
One potential vector of infection that must be managed is the air circulating within the building. Failure to correctly monitor and manage indoor air quality can add cost due to increased lengths of stay, expose the institution to liability, and more importantly, expose patients and staff to unnecessary risk.
In an effective indoor air quality (IAQ) program, an important tool is one that can identify airborne particles, such as the Fluke 985 Air Particle Counter. Used in conjunction with pressure and airflow testers, particle traps and laboratory analysis, the particle counter can provide facilities managers with the data they need to detect IAQ problems, identify and address root causes, and verify when conditions have returned to acceptable levels.
Specifically, a particle counter enables the healthcare facility manager to:
- Document baseline particle counts within a specific space
- Detect when airborne particulate levels diverge from baseline or “normal” levels
- Gain early warning of underlying issues, such as changes in operating procedures, equipment malfunctions, maintenance shortcomings, or failure to separate construction zones from patient areas
- Test particle levels after changes have been made to ensure that remedies have been effective
Sources of IAQ problems in healthcare facilities
The spread of infection through the indoor air is a serious potential problem in healthcare facilities. Such infections can stem from two sources:
- Infectious agents produced by people inside the facility, such as tuberculosis, rubella (measles), and influenza.
- Agents normally present in the human environment that can endanger patients who have compromised immune systems. Such organisms include aspergillus fumigatus, a common species of mold, and others.
Other airborne particulates, such as inorganic materials and allergens, while capable of causing health problems, pose a lesser threat to patients. These contaminants will not be addressed in this article, although the air filtration and air pressure balancing techniques that help control biological pathogens can also control odors, dust, and other non-viable air pollutants.
To control the movement and spread of infectious agents, facility designers and managers establish special purpose spaces called Airborne Infection Isolation (AII) or patient isolation rooms, and Protective Environment (PE) facilities. In both special ventilation spaces, air pressures are regulated to move air from clean to dirty areas.
The AII room would house a patient judged to be a source of airborne infection, such as mycobacterium tuberculosis or measles virus. Vents draw air from the room and exhaust it outside the building. High efficiency particulate air (HEPA) filters may be used to help remove particles from the air. Makeup air flowing into the room is balanced so that the room remains under negative pressure. Thus, the direction of airflow under the door or when the door is opened is into the space, rather than out, helping contain infectious particles.
The PE facility is designed to keep infectious agents out and protect immuno-suppressed patients and others, such as bone-marrow and organ-transplant patients and premature infants, who are especially vulnerable to opportunistic infectious agents. The CDC recommends that PE facilities be maintained under positive air pressure, with directional airflow (from one side of the room, across the patient to the exhaust) and twelve or more air changes per hour. Clean air is supplied through HEPA filters, and point-of-use HEPA filters may also be used. Air flowing through an open door or leak moves out of the space, not in.
Examples of healthcare facility IAQ problems
AII and PE facilities provide a framework for limiting the spread of infectious agents, but they are not foolproof. Building design, inconsistent or inadequate operating procedures, poor maintenance, and facilities construction and renovation projects all have the potential to cause problems. And in any case, protective facilities are not used for all patients.
Even the best air filtration and airflow design can be defeated by inadequate maintenance or incorrect operation. A slipping fan belt on a ventilation supply fan, for instance, could alter the air balance in a protective environment facility, allowing particle-laden air from the hallway outside to flow in. Failure to correctly seal off and ventilate a construction area can send a cloud of construction dust and aspergillus spores into areas where patients are housed. Failure to fix a leaking sink can turn the cabinet below into a nursery for potentially hazardous mold.
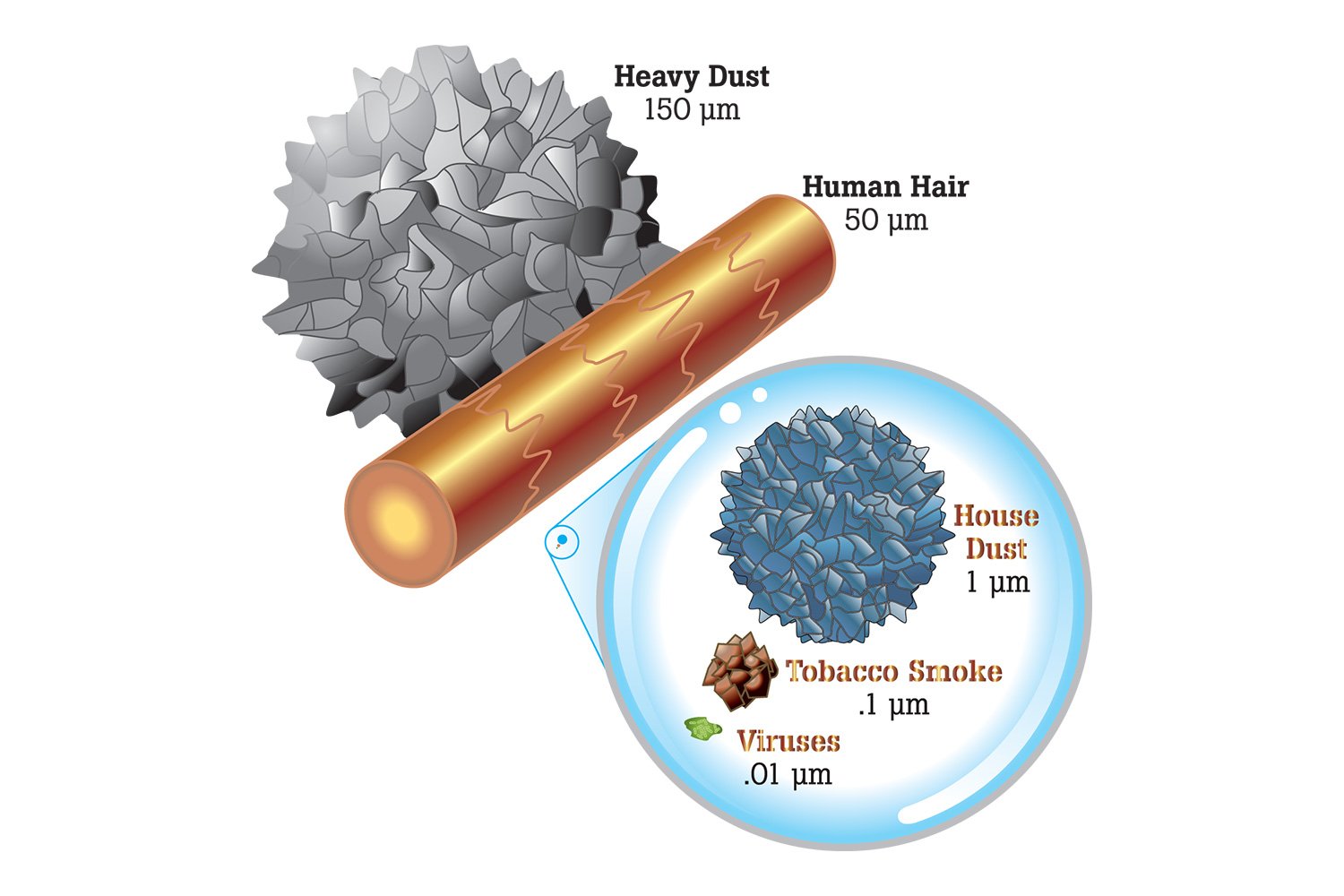
Particulate comparisons: Heavy dust, human hair, house dust, tobacco smoke, and viruses
For example, a hospital environment specialist shared what happened when a cost-conscious hospital administrator turned off the fan ventilating the space over a dropped ceiling in an intensive care unit.
“That allowed humidity to stagnate,” he explained. “When humidity reached extremely high levels that summer, it started raining in the ICU. The water was coming through the ceiling grid and dripping on the patients. They stopped using four or five of the ICU rooms, and diverted patients.”
The larger concern was the possibility that the high humidity would permit mold growth. Raising the room temperature above the dewpoint provided a temporary fix and stopped the “rain.”
Building construction and renovation can pose challenges. Disruption to the building’s envelope, generation of large amounts of construction dust and debris, and the movement of workers and equipment in and out of containment zones all present contamination threats beyond the norm for a healthcare facility. According to the CDC, “an aspergillosis outbreak among oncology patients was attributed to depressurization of the building housing the HSCT unit while construction was underway in an adjacent building. Unfiltered outdoor air flowed into the building through doors and windows, exposing patients in the HSCT unit to fungal spores.”
Contamination testing with airborne particle counters
When such problems occur, an airborne particle counter such as the Fluke 985 can help hospital staff and industrial hygienists detect increased particle levels, identify the sources, and verify the effectiveness of remedial action.
The Fluke 985 Air Particle Counter operates by pumping an air sample of known volume—generally one liter—past a laser beam. As dust particles in the air stream pass through the beam, each one reflects or “scatters” the laser light. A photodetector senses the scattered light and generates an analog electrical signal. Larger particles scatter more light and create higher-voltage electronic “hits.” Onboard electronics track the hits and count the particles in six size categories ranging from .3 to 10 microns (μm). Particles larger than 10 μm generally settle out of the air.
The Fluke 985 can be programmed to take repeat counts instantly or delayed up to 24 hours between samples. It can store 10,000 records of date, time, counts, relative humidity, temperature, sample volumes, alarms, and location label records in its onboard memory. Stored readings may then be downloaded to a computer. As an alternative, the particle counter can be connected directly to a PC for real-time downloads.

Connect your Fluke 985 Particle Counter to a PC for direct, real-time uploading of data
According to the CDC, “particulate sampling (i.e., total numbers and size range of particulates) is a practical method for evaluating the infection-control performance of the HVAC system, with an emphasis on filter efficiency in removing respirable particles (< 5 μm in diameter) or larger particles from the air.
The accuracy, speed, and compact size of the Fluke 985 make it useful for baseline particulate testing, problem detection, and remediation and system maintenance.
- Baseline testing: To know when the “abnormal” occurs, it is necessary to document what are normal levels of particles. It’s not reasonable to expect “clean room” conditions in a healthcare setting. When staff rush into a room to intervene in a patient emergency, there is no time to worry about air quality. Particle counts will soar with the presence of multiple people (human beings shed some 500,000 particles each minute) and medical procedures too can contaminate the air. But later, counts should return to normal or baseline levels. Best practice calls for baseline particulate levels to be documented, both within spaces and in the supply-air flowing into the space.
- Maintenance testing: Once baseline or “normal” particle levels are determined, follow-up tests should be performed and documented periodically. These follow-up tests can provide early warning of developing anomalies and enable the facility manager to intervene before anyone gets sick.
- Filter testing: Used to test for particle levels in the air upstream and downstream from filter media, the Fluke 985 can verify that filters are performing as they should. Testing the level of particles in incoming filtered air at the diffuser (air grate)—air that should be the cleanest in the room—provides an additional check on the performance of filtration systems.
- Locating particle sources: The Fluke 985 can help identify areas where particle counts are elevated and, ultimately, lead the user to the source. A leaking air duct could be sending unfiltered air into a room, for instance; work above a suspended ceiling could be disturbing accumulated dust.
- Verifying the effectiveness of remediation: Once the causes of higher particle counts have been addressed, post-testing will show whether the fixes employed have really worked at bringing particulate levels down.
Controlling airborne contamination within healthcare facilities poses a complex set of challenges far beyond the scope of this article. Numerous additional resources are available to help the professional understand and overcome those challenges. Among those easiest to grasp is the Fluke 985 handheld airborne particle counter.